ONLINE INQUIRY

Fetal Liver Cells Mononuclear Cells 10-12 Weeks Gestation
Cat.No.: CSC-C4500X
Species: Human
Source: Liver
Cell Type: Mononuclear Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
During the 10th to 12th weeks of pregnancy, the primary source of blood production is the foetal liver. Fetal liver mononuclear cells (FLMNCs) play a major immune role in this environment, supporting the foetal immune system. They originate from blood cells in the yolk sac and liver and mainly manifest as mononuclear precursor cells that haven't yet fully transformed into monocytes or macrophages. Morphologically, these cells are relatively large with a nucleus that occupies most of the cell, indicating their immature state. Functionally, these mononuclear cells support the liver's early role in blood formation and assist hematopoietic stem cells (HSCs). In terms of immunity, they participate in initial immune surveillance but are not yet fully mature. As the fetus develops, the composition of cells in the liver changes—the proportion of erythroid cells decreases, while myeloid and lymphoid cells increase. This shift reflects the changing differentiation potential of HSCs and multipotential progenitors, highlighting the fetal liver's vital role in fetal development.
By studying the gene expression, cell-to-cell communication and signalling networks of FLMNCs, scientists can better understand the molecular processes that underlie hematopoiesis and immune development. Such studies contribute to better defining the initial stages of blood and immune diseases, and provide potential therapeutic targets for future interventions. By doing so, scientists could create in vitro and in vivo models of hematopoietic and immune diseases, and then explore more deeply the function of FLMNCs and their role in foetal development.
High CD34 Expression on Human Fetal Liver Mononuclear Cells
Hematopoiesis starts in the foetal liver (FL) at about 5 weeks of gestation and continues until mid-gestation, at which point bone marrow assumes the role. Hematopoietic stem and progenitor cells (HSPCs) from FL can proliferate more efficiently than adult bone marrow and cord blood cells. These cells are used to cure many benign and malignant conditions such as aplastic anemia, acute leukemias, and metabolic diseases. But a few cells from a single foetus is not enough for both laboratory work and clinical testing.
Bhardwaj's team aims to explore methods for expanding fetal liver hematopoietic stem cells in vitro. MNCs were harvested from foetal liver, tagged with the CD34 marker, and maintained in a variety of cytokine combinations on serum-free media to maximise growth and survival. Flowcytometric analysis of foetal liver MNCs revealed a population of CD34 HSPCs ranging from 1.2% to 12.8%, and a median of 5.5%. The peak values of CD34 HSPCs were observed during 8–16 weeks of gestational age (Fig. 1a). From 8 to 10th week, CD34 percentage remained high (8.50 ± 2.4% to 8.70 ± 1.8%); subsequently it started declining. They performed multivariate linear regression analysis on the results which shows that increase in gestational age of 1 week changes CD34 percentage by 0.8463 units. The overall regression model was significant and depicted 1% level of significance with a coefficient of determination value at 0.9429 (Fig. 1b).
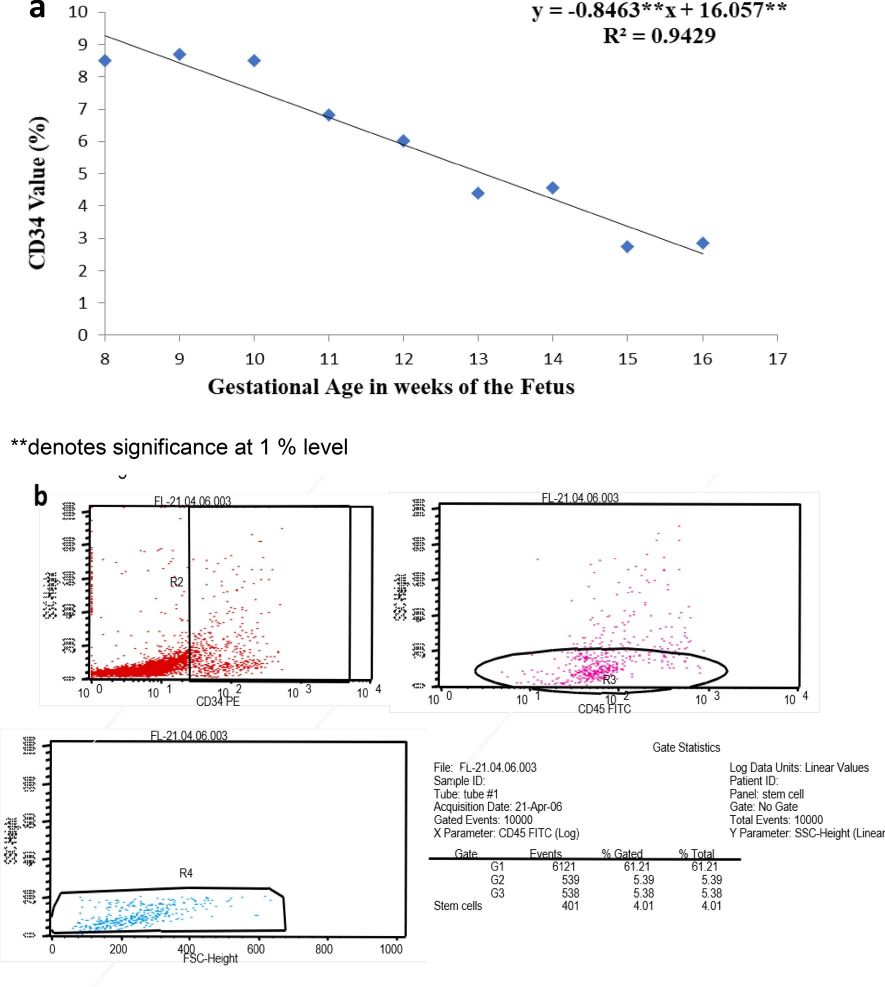 Fig. 1. (a) Percentage of CD34+ cells vs. Gestation age of the fetus. (b) Representative primary immunophenotypic data of CD34+cells from fetal liver mononuclear cells showing 5.39% of total evaluated cells expressing CD34 antigen (Bhardwaj, R., Kumar, L., et al., 2021).
Fig. 1. (a) Percentage of CD34+ cells vs. Gestation age of the fetus. (b) Representative primary immunophenotypic data of CD34+cells from fetal liver mononuclear cells showing 5.39% of total evaluated cells expressing CD34 antigen (Bhardwaj, R., Kumar, L., et al., 2021).
Mean Blood Glucose Levels Decreased after Mixed Transplantation of MSCs and HSCs
Cell therapy can overcome the limitation of conventional treatments (including different medications and β cell replacement) for type 1 diabetes. Based-on several studies human fetal mesenchymal and hematopoietic stem cells are ideal candidates for stem cell therapy. On the other hand, co-transplantation of them can improve their effects. Accordingly, Arjmand et al. explored the utility of co-transplantation of human foetal mesenchymal and hematopoietic stem cells for type 1 diabetes.
They isolated mononuclear cells from foetal liver, centrifuged them on a density gradient, and cultured them in the conditions intended to yield liver-derived mesenchymal stromal cells (hFL-MSCs). CD34 hematopoietic stem cells (CD34 HSCs) were isolated from mononuclear cells using the CD34 microbead kit. Hyperglycemic mice (blood glucose 350 mg/dl) went diabetic five or seven days after STZ administration; their blood glucose averaged over 4,305 mg/dl. These mice were measured for blood glucose each week through animal imaging until day 56. Compared with groups 3 (injected MSCs) and 4 (no stem cell treatment), patients in groups 1 and 2, who received mixed MSCs and HSCs intravenously and/or intrapancreatically, respectively, showed significant decreases in blood glucose 2 weeks after STZ injection and 1 week after transplantation. Furthermore, 7 weeks post transplantation, group 1 and 2 had substantially lower blood glucose levels than groups 3 and 4, and groups 1 and 2 and groups 3 and 4 were undifferentiated in any way (Fig. 2).
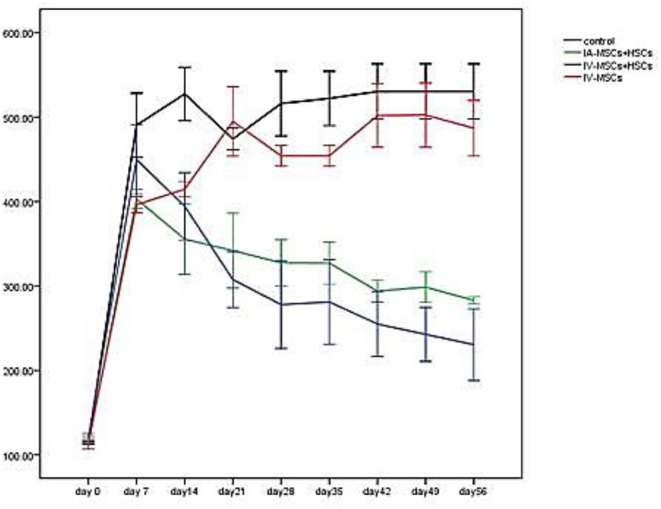 Fig. 2. The mean of blood glucose levels before and after stem cell transplantation in different study group (Arjmand, B., Goodarzi, P., et al., 2019).
Fig. 2. The mean of blood glucose levels before and after stem cell transplantation in different study group (Arjmand, B., Goodarzi, P., et al., 2019).
Ask a Question
Write your own review







