
Human Bronchial Epithelial Cells
Cat.No.: CSC-C4872L
Species: Human
Source: Bronchus
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Never can cryopreserved cells be kept at -20 °C.
Human bronchial epithelial cells (HBECs) are part of the respiratory system, covering the surface of bronchi and comprising a key component of the airway epithelium, which is essential for the functioning of the respiratory system. HBECs have many different cell types, but are most commonly classified into three ultrastructural, functional and biochemical groups: basal, ciliated and secretory cells. Basal epithelial cells are cells found in the basal layer of the bronchial epithelium, typically cone-shaped and small in size. They are stem or primary cells of the epithelial cell layer, responsible for tissue repair and regeneration. Other bioactive molecules emitted by basal epithelial cells include neutral endopeptidase, 15-lipoxygenase derivatives and cytokines. Ciliated epithelial cells are abundant in the bronchial epithelium and columnar, with dense cilia lining the free surface. A cluster of mitochondria around the tip of the cell gives the power to drive the cilia directionally beat in order to flush mucus out of the airways. Secretory (goblet) cells are primarily responsible for releasing mucus and other bioactive materials that are necessary to keep airways moist, shielded and protected. Such cells also release bioactive molecules that have antimicrobial, anti-inflammatory or immunomodulatory effects. In addition, secretory cells have the capacity to self-renew and grow into ciliated epithelial cells. Because of their specialised shape and function, the cultivation of human bronchial epithelial cells provides an excellent vehicle for studying physiological mechanisms of cell proliferation, differentiation, mucus production and ciliary activity. They are therefore a wonderful in vitro model for studying the physiological and pathological functions of the respiratory system.
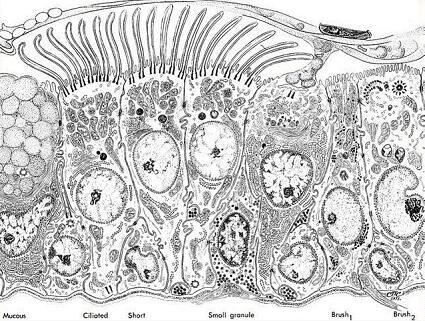 Fig. 1. Illustration of normal human bronchial epithelium (Bucchieri F., 2012).
Fig. 1. Illustration of normal human bronchial epithelium (Bucchieri F., 2012).
Single-Channel Activity in Mitochondria of Human Bronchial Epithelial Cells
Mitochondrial potassium channels, including large-conductance Ca2+-regulated potassium channels (mitoBKca), play crucial roles in maintaining ion homeostasis, affecting mitochondrial respiration, and protecting cells from oxidative stress. Sek et al. demonstrated for the first time the functional properties of mitoBKca in the inner mitochondrial membrane of a human bronchial epithelial cell line. They identified two populations of mitoBKCa channels and the single-channel activity were characterized using the patch-clamp technique.
The first channel's opening probability (Po) increased from 18% at -60 mV to 95% at positive voltages. The second channel had a high Po at all potentials, rising from 72% at negative to 98% at + 60 mV, all in 100 µM Ca2+ (Fig. 1b). Control activity data fitted a Boltzmann function, yielding a V1/2 value of -38.4 mV (Fig. 2b). The control channel was recorded twice as often as the high-activity channel (Fig. 1c). Both were observed in the same mitochondrial isolations, showing no significant conductance differences: control channel at 286.2 ± 5.5 pS and high activity at 287.8 ± 2.8 pS, calculated from the current-voltage relationship (Fig. 2a). Both channels showed no current rectification. Closed and open dwell times were analyzed; high-activity channel closure times were about 1 ms (Fig. 2d), and in the control channel, it decreased from 15 ms at -60 mV to 2 ms at +60 mV (Fig. 2c). Both channel types showed increased open dwell times from -60 to +60 mV, from 4 to 30 ms, consistent with mitoBKca channel behavior.
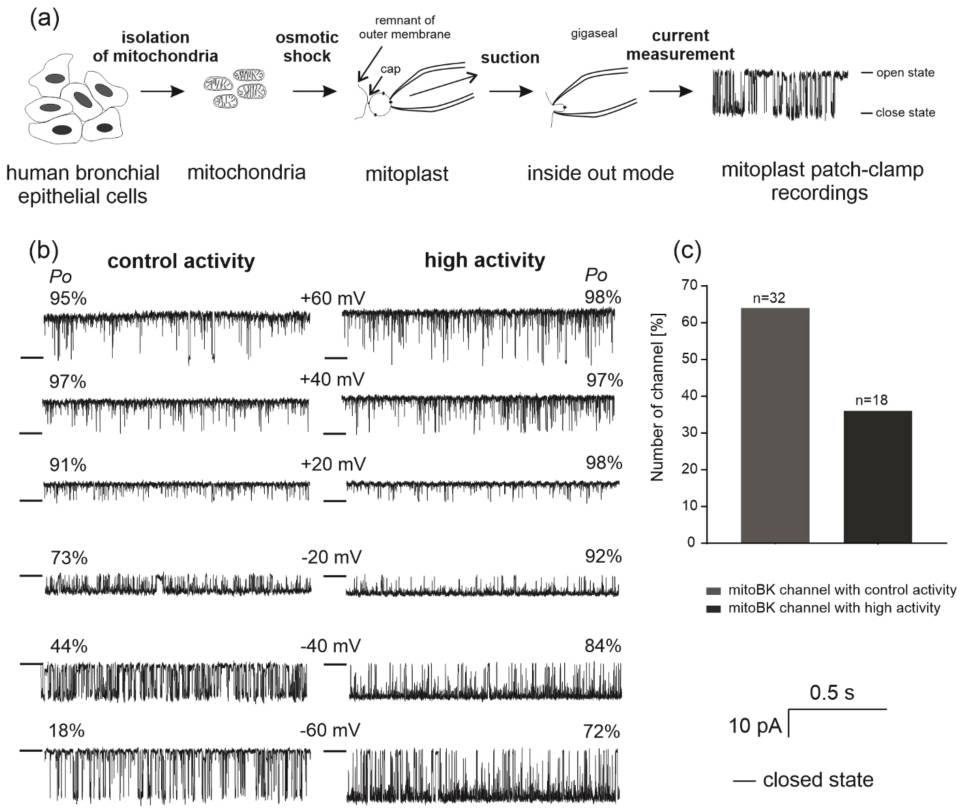 Fig. 1. Outline of the mitochondrial patch-clamp experiments and comparison of the two types of recorded channel activities (Sek A, Kampa RP, et al., 2021).
Fig. 1. Outline of the mitochondrial patch-clamp experiments and comparison of the two types of recorded channel activities (Sek A, Kampa RP, et al., 2021).
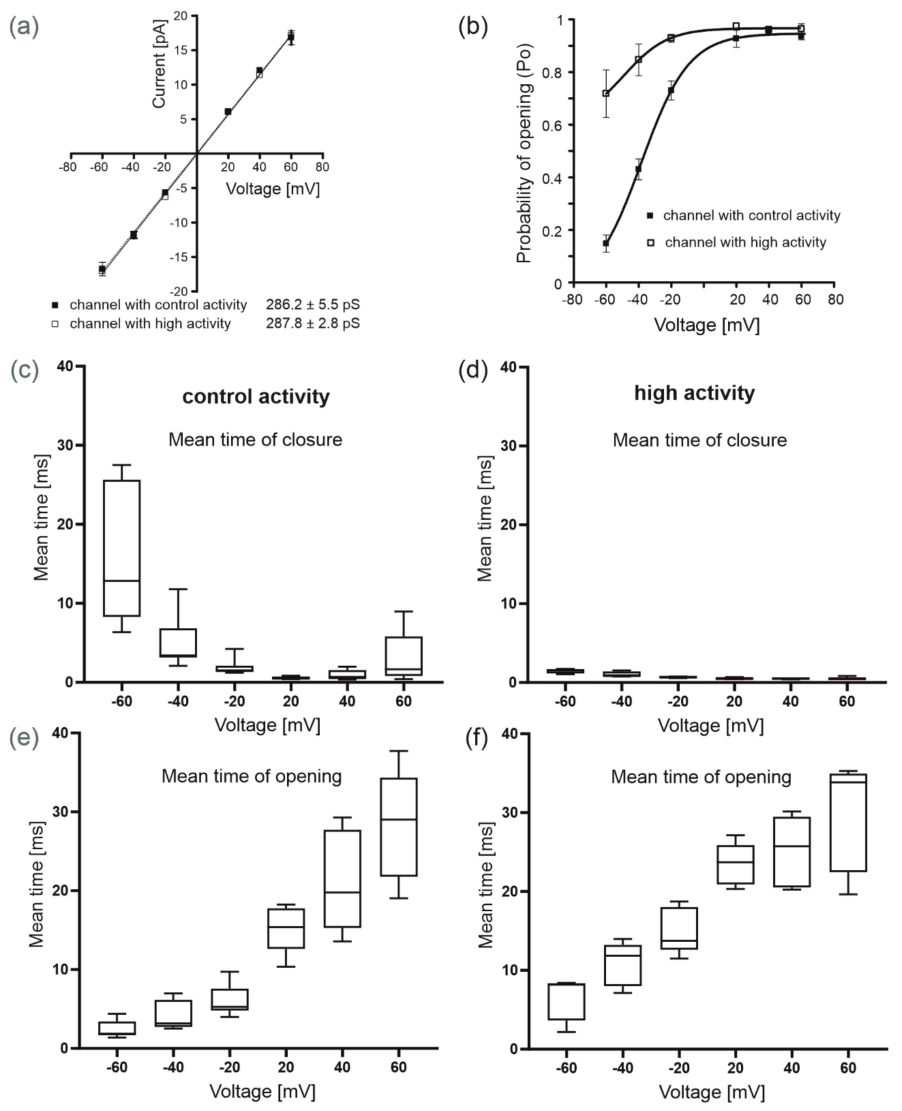 Fig. 2. Biophysical properties of both mitoBKCa channels (channels with control and high activity) present in the inner mitochondrial membranes of human bronchial epithelial cells (Sek A, Kampa RP, et al., 2021).
Fig. 2. Biophysical properties of both mitoBKCa channels (channels with control and high activity) present in the inner mitochondrial membranes of human bronchial epithelial cells (Sek A, Kampa RP, et al., 2021).
ALT Treatment Suppressed CSE-induced Inflammation in Beas-2B and NHBE Cells
Remodeling and inflammation of the airways are hallmarks of COPD. Inflammation, apoptosis and oxidative stress are increased in COPD by smoking cigarettes smoke extract (CSE). Alantolactone (ALT), a sesquiterpene lactone from Inula helenium, has been found to disrupt these processes. Yet it remains unclear exactly how and why ALT plays such an important role in COPD pathology.
Deng et al. evaluated whether ALT reduced inflammation, apoptosis and oxidative stress in human bronchial epithelial Beas-2B cells and normal NHBE cells. They observed that ALT repressed CSE-induced inflammation, apoptosis and oxidative stress by activating the NF-B and Nrf2/HO-1 axises. CSE was infused into Beas-2B and NHBE cells to mimic in vitro pathology of COPD. In Beas-2B and NHBE cells, CSE was significantly higher in concentration (1, 2 and 5% vs. control) than it was in the control group for the following reasons: IL-1, TNF-, IL-6 and IFNY were increased by 24 h at Beas-2B and NHBE cells respectively (Fig. 3A and B). For further studies, they selected the concentration of CSE at 5%. They next tested the role of ALT in CSE-induced inflammation. Compared with the CSE exposure group, ELISA analysis of Beas-2B and NHBE cells confirmed a dose-dependent decrease of IL-1 β, TNF-a, IL-6 and IFN-Y secretion after 1, 5 and 10 μ M ALT exposure (Fig. 3C and D).
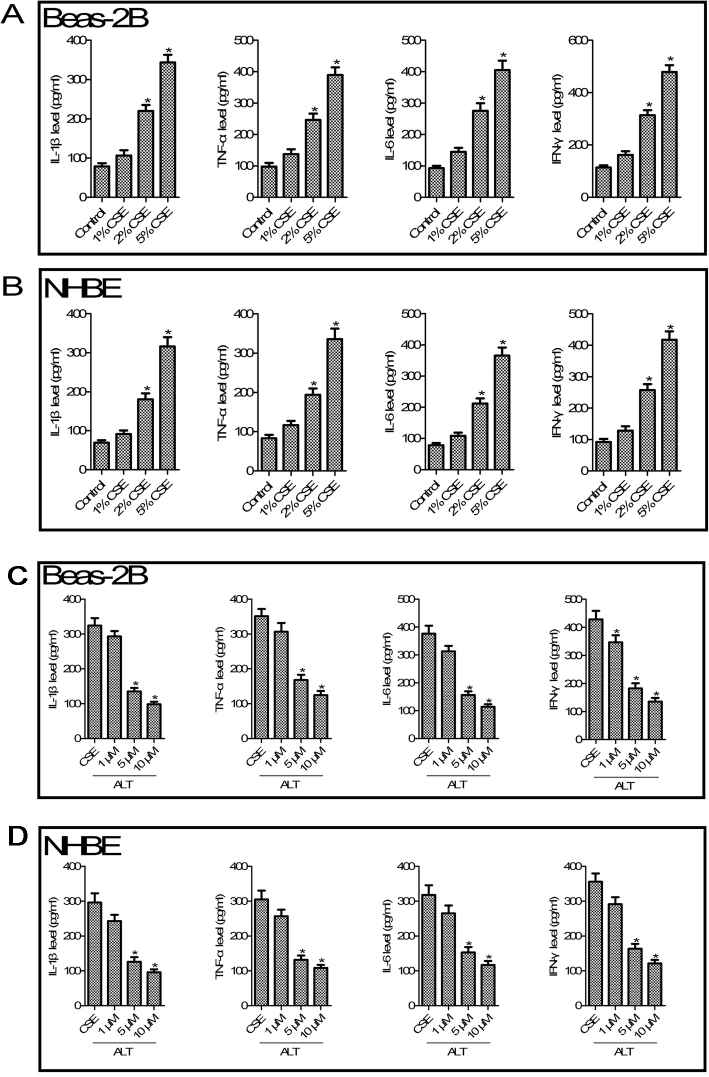 Fig. 3. ALT inhibited CSE induced - IL-1 β, TNF-α, IL-6 and IFN-γ production in human bronchial epithelial Beas-2B and normal bronchial epithelial cells NHBE (Dang, X., He, B., et al., 2020).
Fig. 3. ALT inhibited CSE induced - IL-1 β, TNF-α, IL-6 and IFN-γ production in human bronchial epithelial Beas-2B and normal bronchial epithelial cells NHBE (Dang, X., He, B., et al., 2020).
Our Bronchial Epithelial Cells are also available from Air-Liquid Interface pre-screened, Hypertension, and COPD/Asthma donors.
Creative Bioarray’s Bronchial Epithelial Cells (both normal and diseased) are isolated from the epithelial cells that line the airway of the bifurcation of the lungs and small sections of the bronchia just off of the bifurcation.
It is recommended to use SuperCult® Human Bronchial Epithelial Cell Growth Medium Kit (cat# CM-1351L) for the culturing of Human Bronchial Epithelial Cells.
Microbial infection and pathogenesis; airway inflammation and wound healing; asthma; pulmonary fibrosis, chronic obstructive pulmonary disease; chronic bronchitis; toxicology/other testing of pharmaceuticals.
Ask a Question
Average Rating: 5.0 | 1 Scientist has reviewed this product
Reliable results
The quality and consistency of Creative Bioarray‘s bronchial epithelial cells have significantly enhanced our research results.
23 May 2023
Ease of use
After sales services
Value for money
Write your own review


