ONLINE INQUIRY

Human Renal Glomerular Endothelial Cells
Cat.No.: CSC-C1559
Species: Human
Source: Kidney
Cell Type: Endothelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
HRGEC are isolated from human kidneys. HRGEC are cryopreserved after purification and delivered frozen. Each vial contains >5 x 10^5 cells in 1 ml volume. HRGEC are characterized by immunofluorescent method with antibodies to vWF/Factor VIII and CD31 (P-CAM), and by the formation of microtublar structure in vitro. HRGEC are negative for HIV-1, HBV, HCV, mycoplasma, bacteria, yeast and fungi. HRGEC are guaranteed to expand beyond 15 population doublings at the conditions specified by Creative Bioarray.
The glomerulus, the kidney's central filter, consists of four cell populations: parietal epithelial cells, glomerular endothelial cells (GEnC), visceral epithelial cells (podocytes), and mesangial cells. HRGECs have a unique morphology of tiny transcellular pores, or fenestrations, that extend from 20 to 50 per cent of the endothelial surface. As part of the glomerular microcirculation, HRGECs filter blood. They contribute to the glomerular filtration barrier, along with the glomerular basement membrane and podocytes. This membrane blocks large proteins and blood cells from the filtrate while letting small molecules such as glucose, amino acids, and urea pass through. HRGECs also produce essential bioactive molecules and ramp up this activity under pro-inflammatory and pro-thrombotic conditions. Damage to HRGECs significantly impacts the progression and repair of glomerular diseases.
HRGECs are a useful diagnostic resource in the study of glomerular disorders, including diabetic nephropathy, hemolytic uremic syndrome and pre-eclampsia, where damage is linked to progression of disease. Moreover, given advancements in regenerative medicine, HRGECs could also be used as a cell source to treat glomerular damage.
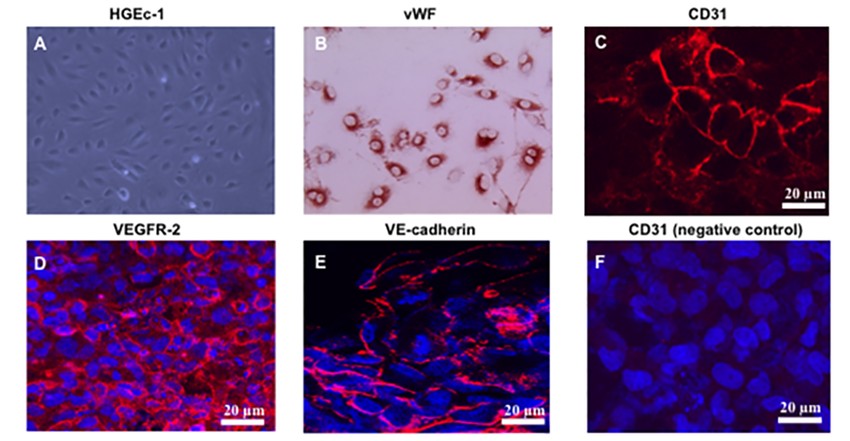 Fig. 1. Characterization of the human glomerular endothelial cell line. Immunofluorescence staining of cultured HGEc-1 for (C) CD31, (D) VEGFR-2, (E) VE-cadherin, all in red color, and (F) human podocytes incubated with the anti- CD31 antibody (Das JR, Gutkind JS, et al., 2016).
Fig. 1. Characterization of the human glomerular endothelial cell line. Immunofluorescence staining of cultured HGEc-1 for (C) CD31, (D) VEGFR-2, (E) VE-cadherin, all in red color, and (F) human podocytes incubated with the anti- CD31 antibody (Das JR, Gutkind JS, et al., 2016).
Establishment of a Microfluidic Glomerular Model Using Human Renal Glomerular Endothelial Cells
Traditional methods for drug nephrotoxicity assessment, such as animal models and static in vitro cultures, often fall short in replicating human responses. To address these limitations, microfluidic technology offers a promising alternative by recreating the dynamic human organ environment with precise control over cell microenvironments.
Qing's team employed a CellASICONIX2 Microfluidic Platform and M04S microfluidic plate for culturing human renal glomerular endothelial cells (HRGECs). Cells were prepared and introduced into the microfluidic plate, which featured multiple inlets and outlets, allowing precise control over the cell environment. After loading, cells were incubated at 37°C with 5% CO2. The microfluidic setup maintained a continuous nutrient supply through gravity-driven medium flow, facilitating cell growth in an environment that closely mimics physiological conditions (Fig. 1A and B). The growth state of the cells in the culture chamber was observed at different times, as shown in Figure 1C. The cells began to grow adherently at approximately day 1, and their morphology varied between round, triangular, fusiform, and irregular. At day 2, the confluence ratio of the cells was greater than 80%. As the incubation time increased, the cells were able to proliferate normally to form a dense cell layer at day 3. The results of live/dead cell staining showed that a well-defined confluent cell monolayer was formed, HRGECs proliferated well in cell chamber (Fig. 1D).
 Fig. 1. Design of a CellASIC-based microfluidic platform to culture glomerular endothelial cells (Qin W, Yang Z, et al., 2022).
Fig. 1. Design of a CellASIC-based microfluidic platform to culture glomerular endothelial cells (Qin W, Yang Z, et al., 2022).
IL-6 Increases Human Renal Glomerular Endothelial Cells Permeability
IgA nephropathy (IgAN) is a common chronic kidney disease that leads to end-stage renal failure. The pathogenesis of IgAN remains unclear, though damage to glomerular endothelial cells is known to contribute to disease progression. An inflammatory cytokine called interleukin 6 (IL-6) is thought to be involved, though its specific role in endothelial cell damage is not clear. Yang's team aims to elucidate the impact of IL-6 on glomerular endothelial cell permeability, by studying an IgAN rat model as well as cultured human renal glomerular endothelial cells (HRGECs).
They used the CCK-8 assay to see whether IL-6 influenced HRGEC permeability. Because it is unclear what IL-6's signaling pathway (classical vs trans-signaling) is, two experimental groups were created: IL-6-none (0, 50, 75, 100, 125, 150 ng/mL) and IL-6 + IL-6 receptor (IL-6R) with increased IL-6. HRGECs were treated for 24 and 48 hours, and proliferation was dramatically reduced at IL-6 levels 125 ng/mL at 48 hours (Fig. 2a). IL-6 plus 15-fold IL-6R resulted in strong inhibition at IL-6 concentrations 75 ng/mL (Fig. 2b), suggesting that IL-6 predominantly functions via the trans-signaling pathway. For further HRGEC stimulation, they then used 100 ng/mL IL-6 and 1500 ng/mL IL-6R and split the samples into normal, IL-6 and IL-6/IL-6R groups. They measured TEER using IL-6 or IL-6/IL-6R, and observed significant decreases in TEER over 24 and 48 hours, while IL-6/IL-6R had a greater impact over 48 hours (Fig. 2c). FITC-dextran tests demonstrated increased permeability in both treated groups, and especially in the IL-6/IL-6R group (Fig. 2d).
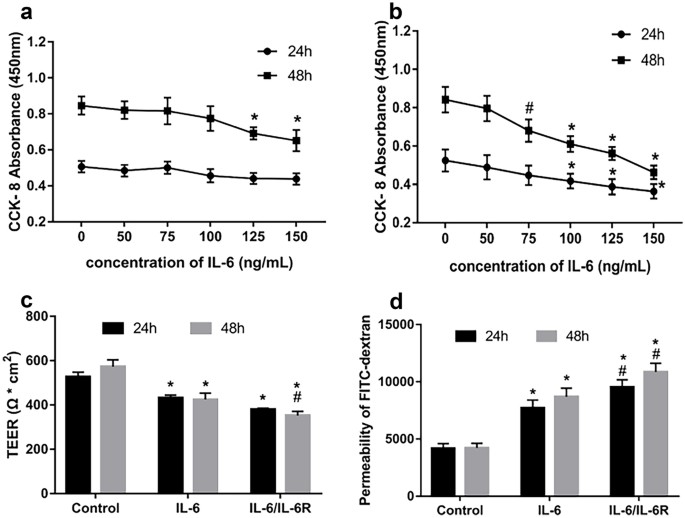 Fig. 2. Effects of IL-6 on HRGEC cell viability and permeability (Yang Y, Fu H, et al., 2022).
Fig. 2. Effects of IL-6 on HRGEC cell viability and permeability (Yang Y, Fu H, et al., 2022).
Ask a Question
Write your own review




