What are Mesothelial Cells?
Mesothelial cells form a monolayer of specialized pavement-like cells that line the body's serous cavities and internal organs. The main function of this layer, called the mesothelium, is to provide a slippery, non-adhesive and protective surface. However, mesothelial cells play other pivotal roles involving transport of fluid and cells across the serosal cavities, antigen presentation, inflammation and tissue repair, coagulation and fibrinolysis and tumor cell adhesion.
Types of Mesothelial Cells
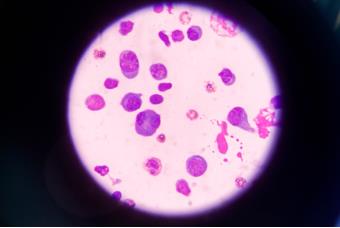
Mesothelial cells are characterized by their flattened and irregular shape and the presence of microvilli on their cell surfaces, which allow efficient fluid transport and reduced friction, and exhibit diversity in their roles and locations within the body. They are divided into different types based on their specific location and the bodily cavity they line, allowing them to contribute uniquely to their respective functions and maintain overall physiological balance throughout the body's complex systems.
Pleural mesothelial cells
Pleural mesothelial cells within the pleural cavity surrounding the lungs play a crucial role in protecting lung function and well-being. This cell population consists of both visceral pleural mesothelial cells covering the lung surface and parietal pleural mesothelial cells situated on the chest wall. Together, they form a dynamic protective shield for the delicate lung environment.
Pericardial mesothelial cells
Pericardial mesothelial cells occupy the pericardial cavity, enveloping the heart, where they serve as essential guardians of cardiac health. These specialized cells contribute significantly to protecting the heart and promoting its smooth, friction-free movement, ensuring the normal functioning of this vital organ.
Peritoneal mesothelial cells
In the peritoneal cavity, encasing the abdominal organs, peritoneal mesothelial cells take on the responsibility of protecting and lubricating the intricate movements of the abdomen. Their presence is essential for maintaining abdominal health and function.
Tunica vaginalis mesothelial cells
The tunica vaginalis mesothelial cells, within the lining of the testes in the scrotum, play a dual role in protecting the testicles and facilitating their movement within this unique anatomical niche. Their presence is essential for maintaining the structural and functional integrity of the testes.
Despite their distinct locations, these mesothelial cells share a common purpose: to establish a protective barrier, secrete serous fluid for lubrication, and facilitate the smooth movement of organs within their respective cavities. This coordinated effort ensures the overall well-being and proper function of the body's systems.
What is the Function of Mesothelial Cells?
Mesothelial cells are specialized and have several specific functions:
Protective barrier and non-adhesive surface
The mesothelium provides a protective barrier against physical damage and invading organisms. Mesothelial cells are tightly bound together by tight junctions, and secrete surface glycosaminoglycans, primarily hyaluronan, which is assembled into hyaluronan-containing pericellular matrixes "coats" around microvilli, protecting the cells from abrasive damage and infective agents. Hyaluronan may also be important in cell differentiation, preventing adhesion formation and tumor cell dissemination. Mesothelial cells also secrete phosphatidylcholine, a major component of lamella bodies and pulmonary surfactant, acting as a lubricant to reduce friction between serosal surfaces.
Antigen presentation
Antigen presentation and T-cell activation are the first steps in generating specific immune response. Human peritoneal mesothelial cells, stimulated by interferon (IFN), induce the proliferation of CD4+ T helper cells in the presence of antigen. Intercellular adhesion molecule-1 (ICAM-1) is the major accessory molecule for antigen presentation by these cells. Mesothelial cells also secrete interleukin (IL)-15 in the presence of IFN.
Tumor cell adhesion and growth
The exact role of mesothelial cells in tumor cell adhesion and growth is unclear. Many studies have shown that the wound mesothelial surface is a privileged site for tumor cell adhesion, possibly due to tumor cells binding to the hyaluronan coat of mesothelial cells, upregulation of adhesion molecules on mesothelial cells in response to inflammatory mediators and exposure of underlying ECM. However, hyaluronan in conditioned medium from cultured mesothelial cells prevented tumor cell attachment to mesothelial cells, possibly by binding to CD44 molecules on tumor cells and preventing their interaction with hyaluronan on the mesothelial cell surface.
Transport of fluid and cells
The mesothelium is actively involved in transport and movement of fluid and cells across the serosal cavities through pinocytic vesicles, intracellular junctions and stomata. Stomata are cavities at the junction of two or more mesothelial cells, 3-12 μm in diameter, and are generally found in those regions where cuboidal mesothelial cells are present. These openings provide a direct access to the underlying submesothelial lymphatic system allowing rapid removal of fluid and cells from the serosal cavities.
Initiation and resolution of inflammation and tissue repair
The balance of pro-, anti- and immunomodulatory mediators regulated by mesothelial cells in serosal tissues is important for the outcome of injury following surgery, infection, or treatments such as CAPD. The correct balance leads to tissue regeneration and re-establishment of normal serosal function; however, loss of this balance can result in increased permeability, oedema, formation of protein rich exudates and ultimately adhesion formation and fibrosis.
Mesothelial cells are involved in initiating and resolving serosal inflammation and repair by secreting various pro-, anti- and immunomodulatory mediators. These include products of the coagulation cascade, chemokines, cytokines and growth factors, prostaglandins and prostacyclin, reactive nitrogen and oxygen species, antioxidant enzymes and extracellular matrix (ECM) molecules. Secretion of chemokines by mesothelial cells promotes directed transmesothelial migration of neutrophils and monocytes, resulting in a massive influx of leukocytes from the vascular compartment into the serosal space. Mesothelial cells also release mediators in response to injury which initiate cell proliferation, migration and ECM synthesis.
Coagulation and fibrinolysis
Mesothelial cells have both procoagulant and fibrinolytic activities. The procoagulant activity is due to tissue factor, the main cellular initiator of the extrinsic coagulation cascade. Fibrin deposition is also aided by the secretion of plasminogen activator inhibitors (PAI), PAI-1 and PAI-2. Fibrinolytic activity is mediated through secretion of tissue plasminogen activator (tPA) and urokinase PA (uPA). The PAs convert the inactive zymogen plasminogen into active plasmin which in turn enzymatically breaks down fibrin. Mesothelial cells are the main source of tPA in serosal cavities but secrete lower levels of uPA.
Creative Bioarray Relevant Recommendations
Accelerate your programs with Creative Bioarray's extensive inventory and prospective network of mesothelial cells.
| Cat. No. | Product Name |
| CSC-7683W | Human Adult Mesothelial Cells |
| CSC-7684W | Human Adult Mesothelial Cells(DIABETIC Donor) |
| CSC-C5367S | Mouse Peritoneal Mesothelial Cells |
| CSC-C5274S | Rabbit Peritoneal Mesothelial Cells |
| CSC-I2097Z | Immortalized Human Mesothelial Cells-SV40 |

