What Is Brain-Targeted Nasal Drug Delivery?
Frontiers in Aging Neuroscience. 2024 Jan 17; 15: 1341295.
Authors: Huang Q, Chen X, Yu S, Gong G, Shu H
INTRODUCTION
The unique anatomical and physiological connections between the nasal cavity and brain provide a pathway for bypassing the blood-brain barrier (BBB) to allow for direct brain-targeted drug delivery through nasal administration. There are several advantages of nasal administration compared with other routes; for example, the first-pass effect that leads to the metabolism of orally administered drugs can be bypassed, and the poor compliance associated with injections can be minimized. Nasal administration can also help maximize brain-targeted drug delivery, allowing for high pharmacological activity at lower drug dosages, thereby minimizing the likelihood of adverse effects and providing a highly promising drug delivery pathway for the treatment of central nervous system diseases.
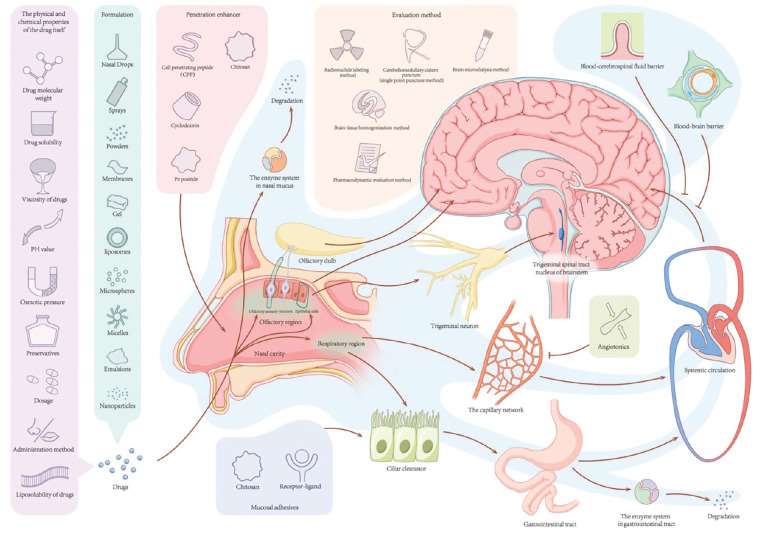 Fig. 1 Schematic diagram of brain-targeted nasal drug delivery.
Fig. 1 Schematic diagram of brain-targeted nasal drug delivery.
Physiological Structure of the Nasal Cavity and Brain
- Physiological structure of the nasal cavity. The human nasal cavity system is a complex structure, with an approximate length of 12-15 cm. It is composed of two cavities, each of which is approximately 7.5 mL in volume, separated by the nasal septum, with an inner surface covered by mucosa; the mucosa is composed of the epithelium and lamina propria and is approximately 150 cm2 in total surface area. The nasal cavity can be divided into three distinct areas based on function and organizational structure, including the vestibular, respiratory, and olfactory areas.
- Relevant physiological structure of the central nervous system (CNS). Three protective capsules surround the brain. The outermost layer is the dura mater, with dural sinuses that contain venous vessels, and the innermost layer is the pia mater. The arachnoid membrane exists between the inner and outer layers, with the cerebrospinal fluid (CSF) flowing in the interstices below it. CSF is produced by the choroid plexus and flows within the ventricles and subarachnoid space, eventually entering the dural sinuses and mixing with venous blood. When the CSF flows through the sieve plates, up to 5% can enter the lamina propria of the olfactory mucosa through the perivascular space near the olfactory filaments before infiltrating into the lymphatic vessels of the nose.
How Drugs Can Enter the Brain Through the Nose?
At present, the precise pathways through which drugs are transported to the brain following absorption across the nasal mucosa remain unclear; however, four main approaches have been identified to date.
| Olfactory nerve pathway | Some studies have shown that most neurophilic viruses (such as rabies, herpetic stomatitis, and equine encephalomyelitis viruses), steroid hormones, metal ions (such as cadmium and nickel), and proteins enter the brain through the olfactory nerve pathway. After crossing the olfactory mucosa, these substances are absorbed at the axon terminals of olfactory neurons through pinocytosis, endocytosis, or simple diffusion. They subsequently flow through the axonal plasma of neurons and are directly transported through the sieve plates to the olfactory bulb, reaching the rhinencephalon. The olfactory nerve pathway is considered to be the most important pathway for the entry of drugs into the brain from the nose, and it represents the most direct pathway for bypassing the BBB. However, axonal transport is relatively slow, the rate of which can vary from 0.1-4 mm/d to 20-400 mm/d depending on the properties of the drug being administered. |
| Olfactory mucosal epithelial pathway | The mucosal epithelial pathway (i.e., the nose-brain pathway) is the route through which drugs reach the olfactory mucosal epithelium and enter the CNS directly via cytosolic action or diffusion. Most small-molecule drugs, such as lidocaine, dopamine, 5-fluorouracil, dihydroergotamine, and insulin, are absorbed into the brain via this pathway. This pathway is further divided into two components, including a transcellular transport pathway and a paracellular pathway; in the former, drug molecules are transported across mucosal epithelia other than olfactory neuron receptor cells via mechanisms involving carrier transport or cytosolic or passive diffusion into supporting and glandular cells surrounding the olfactory nerve. In the latter pathway, drug molecules enter the intercellular fluid through either the interstitial space of the supporting cells or the peripheral cleft between the supporting cells and the olfactory nerve. If the drug molecules transported to the basement membrane are close to the axons in the lamina propria, they will be transported to the CSF within the cells surrounding the neuron. Simultaneously, drugs in the lamina propria may enter the lymphatic and systemic circulation. If the drug molecules transported to the basement membrane pass through the lamina propria, they will enter the space around the olfactory nerve bundle before being transported into the CSF. This pathway is dependent on the anatomical connections between the olfactory submucosa and subarachnoid space. |
| Trigeminal nerve pathway | The ophthalmic and maxillary nerve branches of the trigeminal nerve can extend to epithelial cells in the olfactory and respiratory areas of the nasal cavity, with the opposite end entering the CNS at the pons and terminating at the spinal nucleus of the trigeminal nerve in the brainstem or passing through the ethmoid plate and terminating at the olfactory bulb area. Strong radioactivity was observed in the trigeminal nerve, trigeminal branch ganglia and olfactory bulb following intranasal administration of iodine-125-conjugated insulin-like growth factor 1, with a concentration 10 times higher in the trigeminal nerve than in the olfactory bulb, confirming that, in some cases, the trigeminal nerve may serve as a pathway through which drugs can enter the brain following intranasal administration. |
| Blood circulation pathway | Low-molecular-weight lipophilic drugs predominantly enter the brain following absorption into the general circulation through the rich capillary network in the lamina propria of the respiratory region. However, after entering the general circulation, drugs must cross the BBB to reach the CNS; thus, this pathway is a limiting factor in the therapeutic application of many drugs. |
Factors Affecting Brain-Targeted Nasal Drug Delivery
After a drug is administered via the nose, some of it may enter the CNS directly, whereas some will be absorbed into the general circulation, and some will be removed by the cilia of the nasal mucosa. The amount of drug that can be absorbed through the nasal mucosa is mainly influenced by the physiological characteristics of the nasal cavity, the nature of the drug itself, and factors related to its formulation.
- Physiological properties of the nasal cavity: mechanism of mucociliary clearance, expression of transport proteins, role of enzymes, blood vessel absorption
- Physical and chemical properties of the drug: drug molecular weight, solubility, lipo-solubility, viscosity
Creative Bioarray Relevant Recommendations
| Service/Product Types | Description |
| Administration Routes and Biofluid Sampling | Creative Bioarray offers a variety of administration routes and collection of biological samples, as well as we can provide comprehensive bioanalytical package services. |
| Physicochemical Characterization Assays | Creative Bioarray provides physicochemical characterization assays to help customers accurately evaluate compounds' physicochemical properties such as solubility and stability, reducing drug development difficulties. |
RELATED PRODUCTS & SERVICES
Reference
- Huang Q, et al. (2024). "Research progress in brain-targeted nasal drug delivery." Front Aging Neurosci. 15: 1341295.



