Featured Products
Our Promise to You
Guaranteed product quality, expert customer support

ONLINE INQUIRY
SKM-1
Cat.No.: CSC-6984J
Species: Homo sapiens (human)
Morphology: Round cells growing singly in suspension
Culture Properties: Suspension
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
- Documents
SKM-1 cells are a well-known cell line that was established in 1989 from the peripheral blood of a 76-year-old Japanese man who had been diagnosed with acute monoblastic leukemia (AML) of French-American-British (FAB) subtype M5. The patient had previously experienced myelodysplastic syndromes (MDS), a group of disorders characterized by abnormal blood cell production.
The establishment of SKM-1 cells from a patient with AML following MDS is of particular significance because it allows researchers to study the cellular and molecular characteristics associated with disease progression from MDS to AML. These cells have been widely used in research studies focused on understanding the pathogenesis of AML, investigating therapeutic targets, and exploring potential treatment strategies.
SKM-1 cells exhibit features typically observed in AML, specifically the monocytic subtype (M5). These characteristics include abnormal proliferation, impaired differentiation, and the ability to form colonies in vitro. Researchers have extensively characterized SKM-1 cells, which have contributed to our understanding of the molecular mechanisms underlying AML, as well as drug resistance and therapeutic response.
Metformin Inhibits Cell Proliferation in SKM-1 Cells
Metformin, a widely used antidiabetic drug, has previously been demonstrated to exert anti-cancer effects in certain hematological malignancies. To evaluate the effects of metformin on the proliferation of SKM-1 cells, we performed a CCK-8 assay. As shown in Fig. 1A, metformin at a concentration of 1 mM has little impact on the proliferation at 24 and 48 h but significantly reduces the proliferation at 72 h; when the concentration reaches 5-10 mM, the proliferation is inhibited remarkably from 48 h; metformin at 15-20 mM slows down the proliferation from 24 h. We further detected the effects of metformin on cell apoptosis in SKM-1 cells. The results of flow cytometry (Fig. 1B and C) show that both early and late apoptotic rates of SKM-1 cells in metformin-treated groups (1 mM, 5 mM, 10 mM, 15 mM, 20 mM) are similar to those in the untreated group.
To elucidate the mechanism by which metformin inhibits the proliferation of SKM-1 cells, we performed flow cytometry to evaluate the cell cycle phases at 48 h. As shown in Fig. 2A and B, more SKM-1 cells are arrested at the G1/G0 phase (P < 0.05) in metformin (5 mM, 20 mM) treated groups compared with those in the untreated group. Meanwhile, metformin reduces the expression of CyclinD1 and CDK4 (Fig. 2C and D).
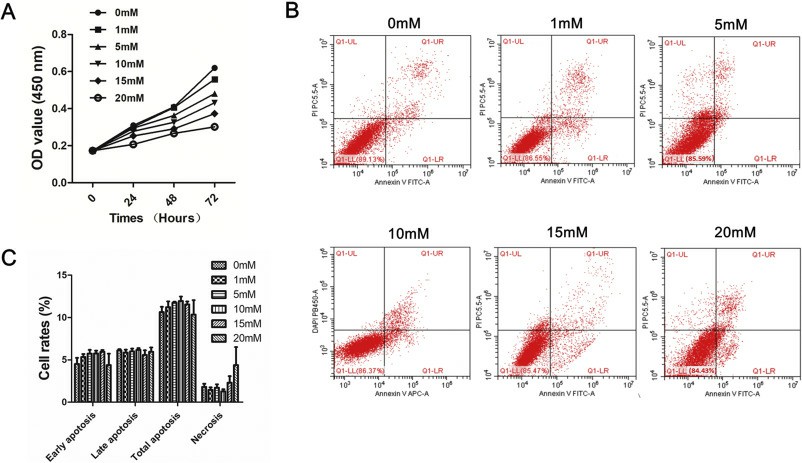 Fig. 1 Metformin inhibits cell proliferation in SKM-1 cells. (Zhou X, et al., 2019)
Fig. 1 Metformin inhibits cell proliferation in SKM-1 cells. (Zhou X, et al., 2019)
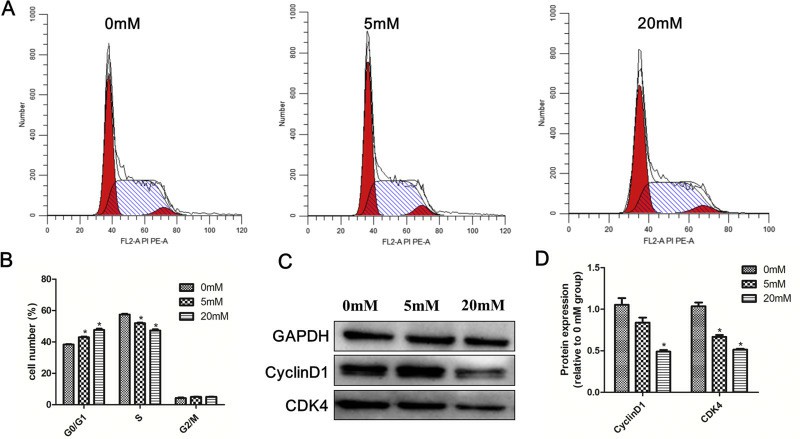 Fig. 2 Metformin induces G0/G1 cell cycle arrest in SKM-1 cells. (Zhou X, et al., 2019)
Fig. 2 Metformin induces G0/G1 cell cycle arrest in SKM-1 cells. (Zhou X, et al., 2019)
Atg3 Overexpression Enhances Bortezomib-Induced Cell Death in SKM-1 Cells
According to a gene expression microarray, atg3 is downregulated in MDS patients progressing to leukemia, but less is known about the function of Atg3 in the survival and death of MSD/AML cells. To explore the function of the Atg3 protein, SKM-1 cells were transfected with a FLAG-tagged ATG3-overexpressing vector or an empty vector lentivirus. At 72 h after transfection, GFP expression was examined using fluorescence microscopy. The transfection efficiency of each group was above 80% (Fig. 3A). The protein expression was further confirmed by Western blotting. The level of the Atg3 protein was significantly greater in the Atg3 overexpression group (Atg3 OE group) than in the control group and mock group (Fig. 3B and 3C, Fig 3D and 3E).
Three groups of cells were treated with different concentrations of bortezomib (1, 10, 50, and 100 nM) for 24 h. The PI-positive rate of each group was dose-dependent. Compared to the control group and mock group, the Atg3 OE group had a statistically significant increased cell death rate (Fig. 4A and 4B). Then, we treated cells of each group with bortezomib at a concentration of 10 nM. At 24 h following treatment, cells of the Atg3 OE group showed nucleolus pyknosis and nuclear fragmentation (Fig. 4C). Similarly, cell growth was significantly inhibited in the Atg3 OE group 24 h following bortezomib treatment (Fig. 4D). These findings suggest that Atg3 significantly enhances bortezomib-mediated cytotoxicity in SKM-1 cells.
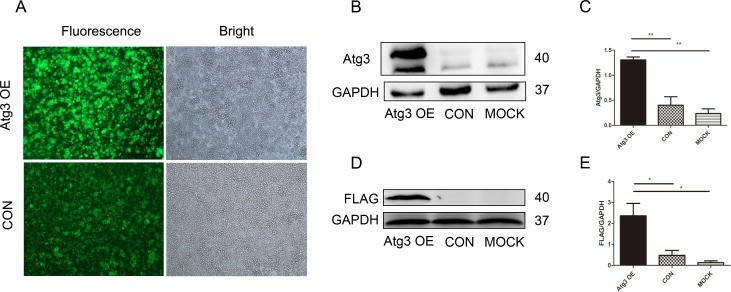 Fig. 3 Lentivirus-mediated Atg3 overexpression in SKM-1 cells. (Zhuang L, et al., 2016)
Fig. 3 Lentivirus-mediated Atg3 overexpression in SKM-1 cells. (Zhuang L, et al., 2016)
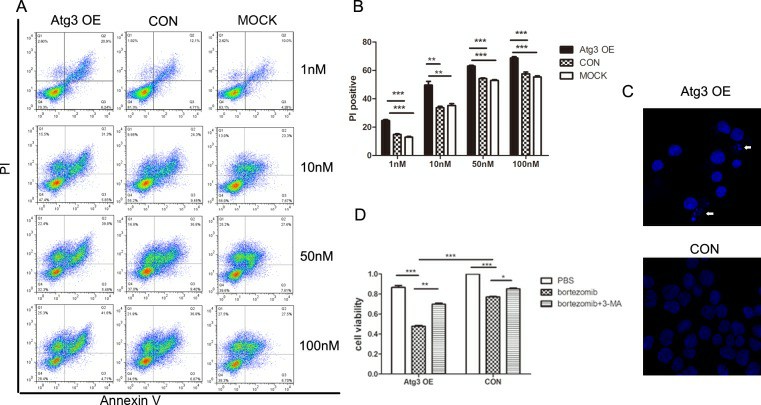 Fig. 4 Upregulation of autophagy by Atg3 overexpression increases the sensitivity of SKM-1 cells to bortezomib treatment. (Zhuang L, et al., 2016)
Fig. 4 Upregulation of autophagy by Atg3 overexpression increases the sensitivity of SKM-1 cells to bortezomib treatment. (Zhuang L, et al., 2016)
There are two types of lymphocytes, T cells, and B cells. And lymphoma occurs when one of these types of lymphocytes grow and multiply uncontrollably. Often, these abnormal cells will build up and cause tumors in the lymph nodes, which are actually present throughout your body.
SKM-1 cells were established in 1989 from the peripheral blood of a 76-year-old Japanese man diagnosed with AML subtype M5. The patient had previously experienced MDS.
SKM-1 cells were established from a patient who had previously experienced MDS. The use of SKM-1 cells allows researchers to study the progression from MDS to acute monoblastic leukemia (AML M5) and investigate the underlying molecular changes associated with disease evolution.
SKM-1 cells provide a valuable model for studying AML treatment resistance. By investigating the behavior and genetic alterations of these cells, researchers can gain insights into the mechanisms underlying drug resistance and identify potential strategies to overcome treatment challenges in AML patients.
Ask a Question
Average Rating: 5.0 | 3 Scientist has reviewed this product
Helpful
The products provided by Creative Bioarray have been very helpful for our cancer research.
15 Nov 2022
Ease of use
After sales services
Value for money
Excellent quality
The SKM-1 cell line obtained from Creative Bioarray was of excellent quality and authenticity.
12 Jan 2024
Ease of use
After sales services
Value for money
Helpful customer support
The customer support team at Creative Bioarray was highly responsive and helpful in addressing my inquiries regarding the SKM-1 cell line.
27 Dec 2023
Ease of use
After sales services
Value for money
Write your own review