Featured Products
Our Promise to You
Guaranteed product quality, expert customer support

ONLINE INQUIRY
EJM
Cat.No.: CSC-C0566
Species: Human
Source: multiple myeloma
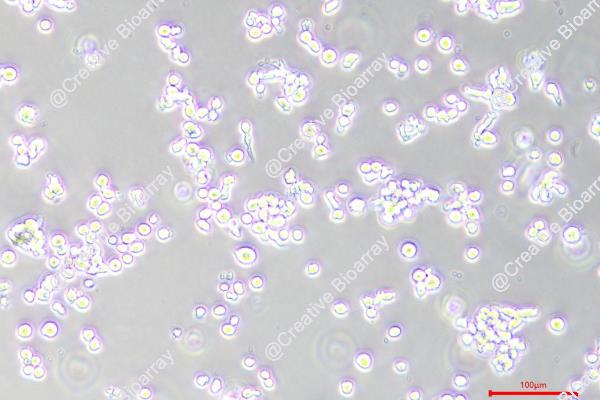
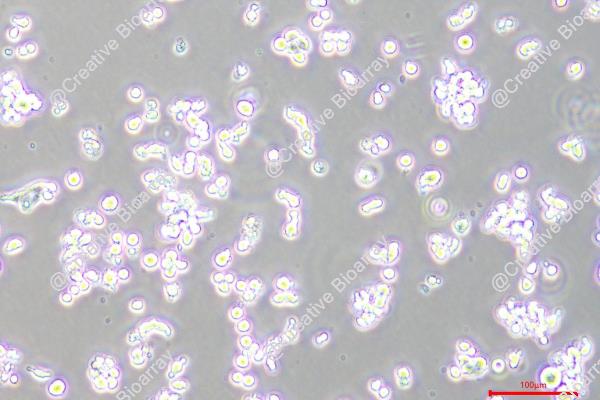
Morphology: round to polymorph, single or clustered cells growing either in suspension or adherent
- Specification
- Background
- Scientific Data
- Publications
- Q & A
- Customer Review
- Documents
Immunology: CD3 -, CD10 -, CD13 -, CD19 -, CD20 -, CD34 -, CD37 +, CD38 +, CD80 -, CD138 +, cyIgG +, cyIgM -, cykappa -, cylambda +
Viruses: PCR: EBV -, HBV -, HCV -, HIV -, HTLV-I/II -, SMRV -
The EJM cell line was established in 1988 from the peritoneal fluid of a 58-year-old woman who was in the terminal refractory stage of IgG lambda myeloma. This cell line has been valuable in research related to multiple myeloma, particularly in studying the characteristics and behavior of myeloma cells in the terminal stage of the disease.
EJM cells have been utilized to investigate various aspects of myeloma biology, including disease progression, response to treatments, and molecular pathways involved in myeloma pathogenesis. Due to their origin from a patient in the refractory terminal stage, EJM cells provide a unique model for studying late-stage myeloma and exploring potential therapeutic strategies for this challenging condition.
Researchers have used the EJM cell line in drug screening, understanding drug resistance mechanisms, and identifying novel treatment approaches targeting refractory myeloma. The insights gained from studies using EJM cells have contributed to advancements in the management of IgG lambda myeloma and have informed the development of new therapeutic interventions for patients with advanced disease.
IGF-I Acting as Growth Factors in Human Multiple Myeloma Cell Lines
Human multiple myeloma (MM) represents a highly aneuploid tumor as shown by cytogenetic studies. This may partly explain the heterogeneity in growth factor requirements demonstrated among MM cells. Several cytokines have been suggested to stimulate the growth of human multiple myeloma (MM) biopsy cells and cell lines. This study investigated the role of insulin-like growth factor I (IGF-I) as a growth and/or survival factor in three MM cell lines: LP-1, EJM, and Karpas 707.
To study the expression of IGF-IR mRNA, RNA was isolated from exponentially growing cells from the MM cell lines LP-1, EJM, and Karpas 707 and performed RT-PCR. As shown in Fig. 1, all cell lines expressed IGF-IR and IGF-I mRNA. To study the effect of IGF-I on the growth of the LP-1, EJM, and Karpas 707 cell lines, cells were incubated with increasing concentrations of IGF-I with or without FBS (Fig. 2). LP-1 (Fig. 2A) cells were stimulated to proliferation in a dose-dependent manner by IGF-I both without and in the presence of 0.5% and 10% FBS. The stimulatory effect was moderate (up to 50%) in the two concentrations of FBS. EJM (Fig. 2B) did not respond to IGF-I in this assay. The Karpas 707 cell line (Fig. 2C) was also growth stimulated by IGF-I both without and in the presence of 0.5% and 10% FBS. The effect is similar to that observed in the LP-1 cultures (up to 45% growth stimulation). Thus, IGF-I can act as a growth factor in human MM.
 Fig. 1 Expression of IGF-IR (left) and IGF-I (right) mRNA in LP-1, EJM, and Karpas 707. (Georgii-Hemming P, et al., 1996)
Fig. 1 Expression of IGF-IR (left) and IGF-I (right) mRNA in LP-1, EJM, and Karpas 707. (Georgii-Hemming P, et al., 1996)
 Fig. 2 Effect of IGF-I on proliferation in LP-1, EJM, and Karpas 707. (Georgii-Hemming P, et al., 1996)
Fig. 2 Effect of IGF-I on proliferation in LP-1, EJM, and Karpas 707. (Georgii-Hemming P, et al., 1996)
Role of IL-16 in Multiple Myeloma
Multiple myeloma is a malignancy characterized by the expansion of a plasma cell clone that localizes to the human bone marrow. Interleukin 16 (IL-16) is involved in regulating the migration and proliferation of normal leukocytes. This study investigated IL-16 expression in cell lines by quantitative reverse transcription-polymerase chain reaction, immunoblot analysis, enzyme-linked immunosorbent assay, flow cytometry, and immunohistochemistry.
IL-16 expression was examined in 10 different multiple myeloma cell lines. Conventional RT-PCR revealed that IL-16 RNA was present in varying amounts in all myeloma cells tested (Fig. 3A). Immunoblot analysis revealed that all 10 cell lines strongly expressed the 80-kDa precursor peptide, pro-IL-16. To confirm the constitutive expression of IL-16 protein in myeloma cell lines at a single-cell level, intracellular staining with a different IL-16 monoclonal antibody was performed followed by flow cytometry. all 10 multiple myeloma cell lines were observed to express intracellular IL-16 protein (Fig. 3B), which was consistent with the RT-PCR and immunoblot findings.
Because IL-16 was present in all of the multiple myeloma cell lines that were available to us, the functional consequences of its overexpression could not be investigated in IL-16-negative lines. Therefore, knockdown experiments were performed using IL-16-specific siRNA. Myeloma EJM and KMS-12-BM cells were transiently transfected with IL-16-targeting siRNA or scrambled sequence control siRNA and the effects on proliferation and apoptosis were evaluated. Two of the three siRNAs resulted in decreased expression of both pro-IL-16 and the mature 20-kDa fragment of IL-16 (Fig. 4A).
Whether siRNA-mediated knockdown of IL-16 expression was examined in EJM and KMS-12-BM cells. Transfection of cells with IL-16 siRNA markedly reduced the proliferation of EJM and KMS-12-BM cells compared with un-transfected cells (Fig. 4E). The anti-proliferative effect of IL-16 knockdown was, at least in part, abrogated by the addition of the recombinant 20-kDa carboxyl-terminal fragment of IL-16 protein, but not by addition of control protein, to the cell culture (Fig. 4E). These findings suggested for the first time that IL-16, in particular its carboxyl-terminal fragment, might be an important growth factor for myeloma cells.
 Fig. 3 IL-16 expression in myeloma cell lines EJM and KMS-12-BM. (Atanackovic D, et al., 2012)
Fig. 3 IL-16 expression in myeloma cell lines EJM and KMS-12-BM. (Atanackovic D, et al., 2012)
 Fig. 4 Functional consequences of IL-16 expression in myeloma cell lines, EJM and KMS-12-BM. (Atanackovic D, et al., 2012)
Fig. 4 Functional consequences of IL-16 expression in myeloma cell lines, EJM and KMS-12-BM. (Atanackovic D, et al., 2012)
The six primary steps in the immunomagnetic separation of Cryptosporidium: 1) addition of immunoblasts, 2) capture of oocysts and cysts by beads, 3) magnetic separation of immunocomplex formed from debris, 4) discarding of waste, 5) acid dissociation of bead immunocomplex and 6) concentration of oocysts/cysts left in the tube.
EJM cells are commonly used as a model system for studying IgG lambda myeloma, providing insights into disease mechanisms, drug responses, and potential therapeutic approaches.
EJM cells express the IgG lambda immunoglobulin subtype, as indicated by the IgG lambda myeloma diagnosis.
The specific research findings or characteristics associated with EJM cells would depend on the studies conducted on these cells. It is recommended to refer to published research articles or studies that have utilized EJM cells for detailed information.
Ask a Question
Average Rating: 5.0 | 3 Scientist has reviewed this product
Wide-range of applications
Creative Bioarray has a wide range of cell products that can help with more experimental topics such as tumor progression, metastasis, drug resistance, and immune response.
20 Dec 2022
Ease of use
After sales services
Value for money
Comprehensive documentation
The cells arrived in excellent condition, and the provided documentation and protocols were comprehensive, making it easy to handle and culture them.
10 Jan 2024
Ease of use
After sales services
Value for money
Highly recommend!
I would highly recommend Creative Bioarray's EJM cell products to researchers studying myeloma or related fields.
17 Oct 2023
Ease of use
After sales services
Value for money
Write your own review
- You May Also Need