- You are here: Home
- Disease Models
- Cardiovascular Disease Models
- Pulmonary Arterial Hypertension (PAH) Models
- Chronic Hypoxia-Induced Pulmonary Arterial Hypertension (PAH) Model
Disease Models
- Oncology Models
-
Inflammation & Autoimmune Disease Models
- Rheumatoid Arthritis Models
- Glomerulonephritis Models
- Multiple Sclerosis (MS) Models
- Ocular Inflammation Models
- Sjögren's Syndrome Model
- LPS-induced Acute Lung Injury Model
- Peritonitis Models
- Passive Cutaneous Anaphylaxis Model
- Delayed-Type Hypersensitivity (DTH) Models
- Inflammatory Bowel Disease Models
- Systemic Lupus Erythematosus Animal Models
- Asthma Model
- Sepsis Model
- Psoriasis Model
- Atopic Dermatitis (AD) Model
- Scleroderma Model
- Gouty Arthritis Model
- Carrageenan-Induced Air Pouch Synovitis Model
- Carrageenan-Induced Paw Edema Model
- Experimental Autoimmune Myasthenia Gravis (EAMG) Model
-
Cardiovascular Disease Models
- Surgical Models
- Animal Models of Hypertension
- Venous Thrombosis Model
- Atherosclerosis model
- Cardiac Arrhythmia Model
- Hyperlipoidemia Model
- Doxorubicin-induced Heart Failure Model
- Isoproterenol-induced Heart Failure Model
- Arterial Thrombosis Model
- Pulmonary Arterial Hypertension (PAH) Models
- Heart Failure with Preserved Ejection Fraction (HFpEF) Model
-
Neurological Disease Models
- Alzheimer's Disease Modeling and Assays
- Seizure Models
- Parkinson's Disease Models
- Ischemic Stroke Models
- Acute Spinal Cord Injury (ASCI) Model
- Traumatic Brain Injury (TBI) Model
- Hypoxic-Ischemic Encephalopathy (HIE) Model
- Tourette Syndrome (TS) Model
- Amyotrophic Lateral Sclerosis (ALS) Model
- Huntington's Disease (HD) Model
- Intracerebral hemorrhage (ICH) Models
- Pain Models
- Metabolic Disease Models
- Liver Disease Models
- Rare Disease Models
- Respiratory Disease Models
- Digestive Disease Models
-
Urology Disease Models
- Cisplatin-induced Nephrotoxicity Model
- Unilateral Ureteral Obstruction Model
- 5/6 Nephrectomy Model
- Renal Ischemia-Reperfusion Injury (RIRI) Model
- Diabetic Nephropathy (DN) Models
- Passive Heymann Nephritis (PHN) Model
- Adenine-Induced Chronic Kidney Disease (CKD) Model
- Kidney Stone Model
- Doxorubicin-Induced Nephropathy Model
- Orthopedic Disease Models
- Ocular Disease Models
- Skin Disease Models
- Infectious Disease Models
Chronic Hypoxia-Induced Pulmonary Arterial Hypertension (PAH) Model
Creative Bioarray has amassed a wealth of experience and expertise in the realm of pulmonary arterial hypertension (PAH) research. Our commitment to innovation and precision has led to the successful establishment of a hypoxia-induced PAH model, meticulously designed to simulate the conditions of the disease in order to rigorously evaluate the efficacy of drug candidates. This model provides an invaluable platform for our clients to screen and refine potential therapeutic agents, thereby accelerating the drug development process for PAH treatments.
Hypoxia stands as the preeminent model employed in the exploration of pulmonary vascular remodeling, a critical aspect of PAH research. The pathophysiology of hypoxia-induced PAH is marked by profound vascular remodeling, which predominantly manifests as the narrowing of arteries due to structural changes, as opposed to the transient constriction of vessels. This remodeling process is intricate and multifaceted, encompassing a spectrum of biological events. These include the dysfunction of endothelial cells, the acquisition of muscular layers by typically non-muscular pulmonary arteries, the transformation and proliferation of vascular smooth muscle cells (VSMCs), an upsurge in the deposition of extracellular matrix, and the phenomenon of erythrocytosis. Together, these processes contribute to the thickening of vessel walls, leading to increased resistance to blood flow and the subsequent development of PAH. The hypoxia-induced model thus provides a vital platform for dissecting the complex mechanisms underlying pulmonary vascular pathology and for the development of targeted therapeutic strategies.
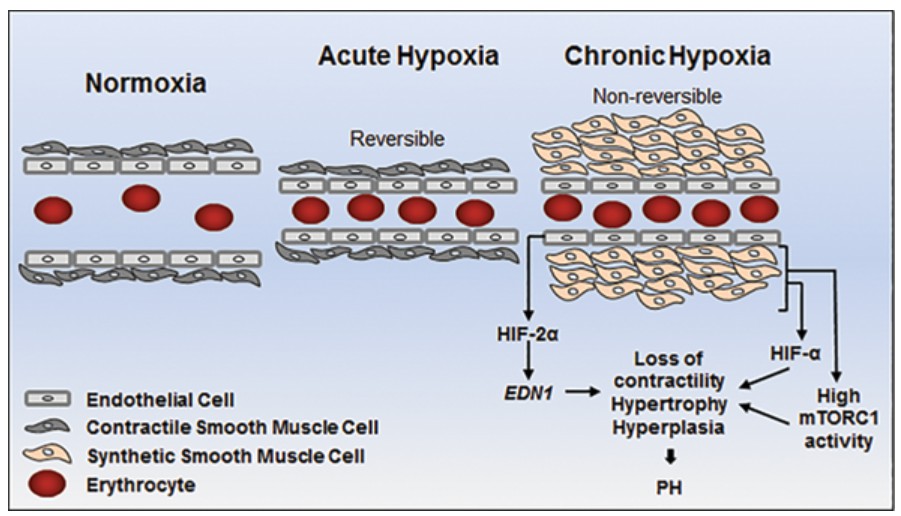 Fig. 1 Schematic representation of pulmonary arterial responses to normoxia, acute hypoxia and chronic hypoxia. (Charolidi et al. 2017)
Fig. 1 Schematic representation of pulmonary arterial responses to normoxia, acute hypoxia and chronic hypoxia. (Charolidi et al. 2017)
Our Chronic Hypoxia-Induced Pulmonary Arterial Hypertension (PAH) Model
- Available Animal
- Rat
- Mouse
- Modeling Method
Male rats are randomly divided into two groups: the normoxia group and the hypoxia group. Rats in the normoxia group are kept in a normoxia environment for 4 weeks, while rats in the hypoxia group are kept in a hypoxic chamber (10% O2). At the end of 4 weeks, the heart function was assessed by echocardiography.
- Endpoints
- Right ventricular systolic pressure (RVSP)
- Right ventricular hypertrophy index (RVHI)
- Body weight
- Tissue weight: heart, lung
- Histology analysis (lung tissue): H&E staining, Sirius red staining, Masson trichrome staining, etc
- qPCR or Western blot
- Other customized endpoints
Example Data
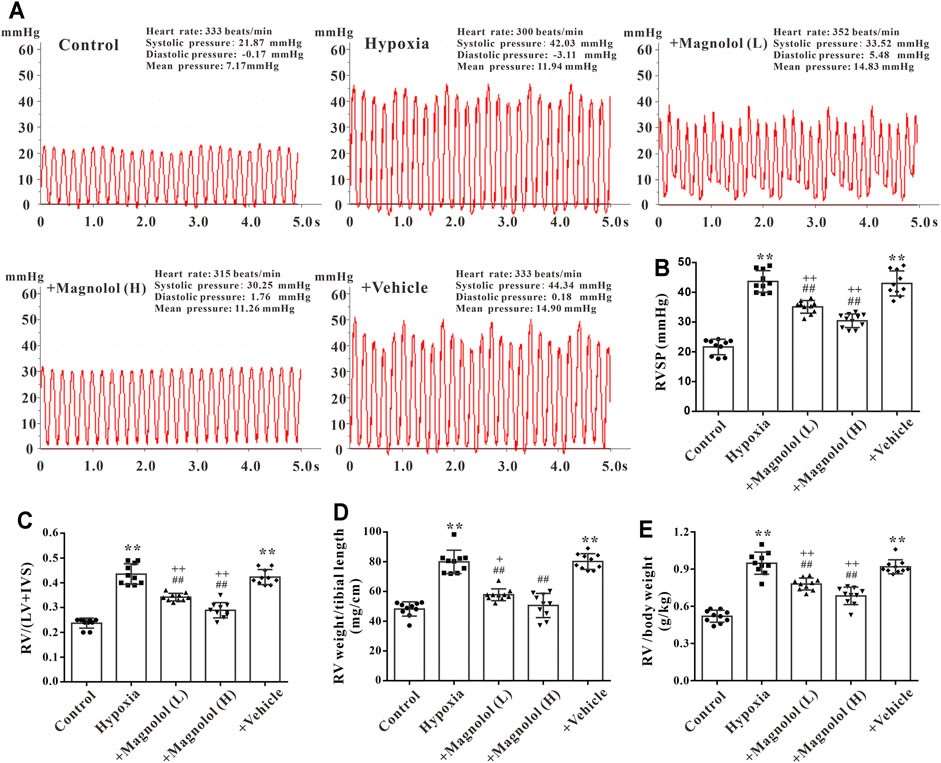 Fig. 2 Magnolol prevented hypoxia-induced PAH and RV remodeling. (A) Representative images for right ventricular systolic pressure (RVSP) were measured by the right heart catheterization method. (B) The value of RVSP in each group. (C) The ratio of RV weight to left ventricular (LV) plus interventricular septum (IVS). (D) The ratio of RV weight to tibial length. (E) The ratio of RV weight to body weight. (Fu et al. 2021)
Fig. 2 Magnolol prevented hypoxia-induced PAH and RV remodeling. (A) Representative images for right ventricular systolic pressure (RVSP) were measured by the right heart catheterization method. (B) The value of RVSP in each group. (C) The ratio of RV weight to left ventricular (LV) plus interventricular septum (IVS). (D) The ratio of RV weight to tibial length. (E) The ratio of RV weight to body weight. (Fu et al. 2021)
Meanwhile, we also provide another PAH model that maybe you are interested in:
Quotation and Ordering
Creative Bioarray offers fast and affordable services to our clients while maintaining the highest levels of quality and accuracy. We take pride in utilizing our expertise to assist our clients in enhancing their drug development endeavors. If you are interested in our services, please feel free to contact us at any time or submit an inquiry to us directly.
References
- Charolidi, N., Carroll, V.A. Hypoxia and Pulmonary Hypertension [Internet]. Hypoxia and Human Diseases. InTech, 2017.
- Fu, M., et al. Magnolol attenuates right ventricular hypertrophy and fibrosis in hypoxia-induced pulmonary arterial hypertensive rats through inhibition of the JAK2/STAT3 signaling pathway. Frontiers in pharmacology, 2021, 12: 755077.
- Wu, X.H., et al. Experimental animal models of pulmonary hypertension: Development and challenges. Animal Model Exp Med, 2022; 5(3):207-216. doi:10.1002/ame2.12220
For research use only. Not for any other purpose.

